Mumps is a contagious viral disease that has affected human populations for centuries.
While many people today think of it as a childhood illness of the past, especially in countries with widespread vaccination programs, mumps still causes outbreaks when conditions allow.
This has been confirmed by a recent surge of cases in Keta Township in the Volta Region of Ghana, where around 50 people have reportedly been affected.
What Is Mumps?
Mumps is caused by the mumps virus, a member of the Paramyxoviridae family. The virus primarily attacks the salivary glands, especially the parotid glands near the jaw and ears.
The hallmark symptom is painful swelling of one or both of these glands. Other symptoms can include fever, headache, muscle aches, fatigue, and loss of appetite.
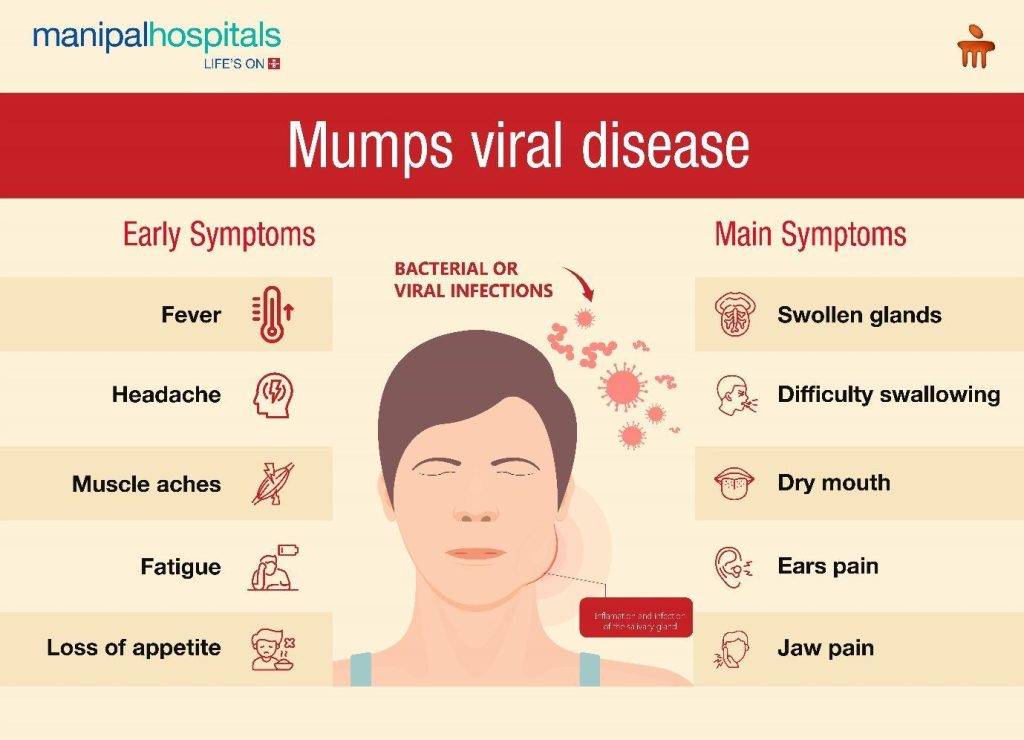
Credit: Manipal Hospitals
In the Keta outbreak, for instance, health officials spotted the typical symptoms, including facial swelling, fever, headache, and muscle aches, among those affected.
Historical Background and Vaccination
Before the development of the mumps vaccine in the mid-20th century, mumps was a common disease worldwide, causing regular outbreaks in schools and crowded communities. The MMR vaccine (Measles, Mumps, Rubella) dramatically reduced cases in countries with high vaccine coverage.
Despite this success, mumps has not been completely eradicated. Outbreaks still occur, even in highly vaccinated populations. This is partly because the vaccine, while effective, does not provide lifelong immunity for everyone. Over time, immunity can wane, leaving adolescents and young adults susceptible to infection.
How Mumps Outbreaks Occur
A mumps outbreak begins when the virus enters a community with enough susceptible individuals, typically unvaccinated people or those whose immunity has waned. The virus can be brought into a community via travellers who are infected but not yet symptomatic.
READ ALSO: Reducing High Rate Of Blood Pressure Among The Youth
Mumps has an incubation period, usually about 16 to 18 days, during which a person can spread the virus without knowing they are sick.
Outbreaks are especially common in settings where people are in close contact for extended periods. Universities, boarding schools, military barracks, refugee camps, and correctional facilities are examples of environments where mumps can spread rapidly. Even in populations with high vaccination coverage, close contact can overwhelm partial immunity and allow transmission to occur.
Modes of Transmission
Mumps spreads primarily through respiratory droplets. When an infected person coughs, sneezes, talks, or shares utensils, the virus can be transmitted to others. It can also spread through direct contact with saliva or contaminated surfaces. Because the virus can survive for a short time on objects, shared items such as cups, bottles, and eating utensils can contribute to transmission.
Individuals with mumps are most contagious from a few days before the onset of symptoms to about five days after parotid gland swelling begins. This makes containment difficult, as people often spread the virus before realising they are sick.
Symptoms and Clinical Presentation
Many people infected with mumps experience mild or even no symptoms, yet they can still spread the virus. When symptoms appear, they typically include:
- Fever, headache, and fatigue.
- Swollen, painful parotid glands (one or both sides of the face).
- Loss of appetite

Complications Associated with Mumps
Although mumps is often mild, it can cause serious complications, particularly in older children and adults. One of the most well-known complications is orchitis, an inflammation of the testicles, which can occur in post-pubertal males. While orchitis rarely leads to infertility, it can cause significant pain and, in rare cases, reduced fertility.
Other complications include oophoritis (inflammation of the ovaries) in females, meningitis (inflammation of the membranes surrounding the brain and spinal cord), encephalitis (brain inflammation), pancreatitis, and hearing loss. Permanent hearing loss, although rare, is one of the most serious potential outcomes of mumps infection.
Public Health Response to Mumps Outbreaks
When a mumps outbreak is identified, public health authorities take several steps to control its spread. Surveillance systems are used to detect and confirm cases, often through laboratory testing of saliva or blood samples.
Confirmed cases are usually advised to isolate for at least five days after the onset of gland swelling to reduce transmission.
Contact tracing may be conducted to identify individuals who have been exposed to the virus. In outbreak settings, health authorities often recommend additional doses of the MMR vaccine for people at increased risk, such as students in affected universities.
This strategy, sometimes referred to as a “third dose” during outbreaks, has been shown to help control transmission in certain settings.
The Role of Vaccine Hesitancy
Vaccine hesitancy has contributed to the resurgence of mumps in some regions. Misinformation, fear of side effects, and lack of access to healthcare can lead to lower vaccination rates, creating pockets of susceptibility. When vaccination coverage falls below a certain threshold, herd immunity weakens, making outbreaks more likely.
Even in communities with high overall vaccination rates, uneven distribution of immunity can allow outbreaks to occur. This highlights the importance of maintaining consistently high vaccine coverage across all population groups.
Prevention and Control Measures
Vaccination remains the most effective way to prevent mumps and control outbreaks. The MMR vaccine is safe and highly effective at reducing the severity and spread of the disease.
In addition to vaccination, good hygiene practices play an important role. Regular handwashing, covering the mouth and nose when coughing or sneezing, and avoiding sharing personal items can help reduce transmission.
During outbreaks, public awareness campaigns are often used to educate people about symptoms and encourage early medical consultation.
Schools and institutions may implement temporary measures such as isolating infected individuals, reducing large gatherings, or enhancing cleaning protocols.
Conclusion
In a nutshell, the outbreak of mumps disease serves as a reminder that infectious diseases can re-emerge even in the era of modern medicine. While vaccination has dramatically reduced the global burden of mumps, the disease has not disappeared.
Factors such as waning immunity, close-contact environments, international travel, and vaccine hesitancy all contribute to the persistence of outbreaks.
Effective control of mumps outbreaks requires a combination of strong vaccination programs, rapid public health response, community cooperation, and accurate information.
















